 Shoulder disorders and complaints constitute an important health problem and affects 18-26% of adults at any point in their life ,making it one of the most common regional pain syndromes . Symptoms can be persistent and disabling in terms of an individual’s ability to carry out daily activities both at home and in the workplace.
Shoulder disorders and complaints constitute an important health problem and affects 18-26% of adults at any point in their life ,making it one of the most common regional pain syndromes . Symptoms can be persistent and disabling in terms of an individual’s ability to carry out daily activities both at home and in the workplace.
The shoulder is made to withstand heavy physical demands and to do so over an unusually wide range of motion. To achieve this, it is not a simple ‘ball and socket’ joint but rather a complex composed of four articulations and a supporting arrangement of bones, muscles and ligaments within and outside of the joint capsule. However, its complexity and the nature of the demands on it, make it susceptible to a range of articular and peri-articular pathologies.
Common shoulder disorders
- Subacromial impingement syndrome.
- Tendinopathy of the biceps tendon.
- Rotator cuff tears.
- Frozen shoulder.
Individual risk factors
- Female gender.
- Obesity.
- Smoking.
- Older age.
- Co-existing medical disorders (eg inflammatory arthritis, polymyalgia rheumatica, fibromyalgia, multiple sclerosis, diabetes mellitus ).
Occupational mechanical risk factors
- Manual handling (heavy lifting, pushing, pulling, holding, carrying.
- Highly repetitive work.
- Vibration.
- Repeated or sustained shoulder postures with >60 flexion or abduction.
Forceful exertions, a high level of static contractions, prolonged static loads, and extreme postures ,as well as combinations of these factors.
Psychosocial risk factors
- Job insecurity.
- Low job control.
- High job demands.
- Poor support from supervisors and colleagues.
Job title and shoulder disorders
Job title - Fish processing workers.
- Shipyard welders.
- Slaughterhouses workers.
- Meat processing workers.
- Fishermen.
- Workers using vibrating tools.
- Drivers.
- Teachers.
- Supermarket cashiers.
- Hairdressers.
Subacromial impingement syndrome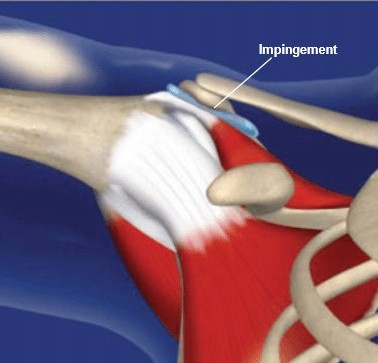
Subacromial Impingement Syndrome is the commonest disorder of the shoulder, accounting for 44%–65% of all complaints of shoulder pain. SAIS encompasses a spectrum of subacromial space pathologies including partial thickness rotator cuff tears, rotator cuff tendinosis, calcific tendinitis, and subacromial bursitis. The main consequences of SAIS are functional loss and disability .
Shoulder impingement results from an “inflammation and degeneration of the anatomical structures in the region of the subacromial space”. The subacromial space is defined by the humeral head inferiorly, the anterior edge and under surface of the anterior third of the acromion, coracoacromial ligament, and the acromioclavicular joint superiorly. As the arm is abducted or rotated, the subacromial space width changes and the humerus gets closer to the anteroinferior edge of the acromion. This is true especially at 90° of abduction and 45° internal rotation of the shoulder.
If the fine balance that regulates the shoulder kinematics is compromised, the humeral head migrates superiorly and the bursa protecting the rotator cuff, as well as the cuff itself becomes increasingly compressed.
Neer was also one of the first to classify the impingement lesions and described three stages depending on the amount of damage in the subacromial space and the age of the patient.
Stages according to Neer
- Stage 1: Edema and hemorrhage, age <25 years, reversible.
- Stage 2: Fibrosis and tendinitis, age 25–40 years, recurrent pain with activity.
- Stage 3: Bone spurs and tendon rupture, age >40 years, progressive disability.
Etiology
- Anatomical Factors
- Hooked (type III)acromion.
- Thickening of the coracoacromial ligament.
- Biomechanical Factors
- Dynamic narrowing of the subacromial space
- Posterior Capsule
- Posterior capsular tightness
- Scapular Musculature
- Aberrant scapular muscle activity may lead to abnormal scapular kinematics.
- Spine
- A relatively small increase in thoracic spine flexion has resulted in a more elevated and anteriorly tilted scapula at rest, and less upward rotation and posterior tilt during glenohumeral elevation. This results in a secondary impingement syndrome
- Rotator Cuff Musculature
- Weakness or dysfunctional rotator cuff musculature can lead to changes in glenohumeral and scapulothoracic kinematics.
Diagnosis
Accurate diagnosis of SIS is made by an accurate history, careful examination, and analysis of relevant investigations.
History and clinical examination
Pain related to this syndrome is often described to be an anterolateral arm pain . Pain on abduction of the shoulder between 60° and 120° is referred to as the painful arc and may indicate the presence of SIS.
Clinical Tests
The combination of the Neer's and Hawkins–Kennedy test, painful arc sign, and weakness in external rotation was most likely to pick up the syndrome. It is important to exclude other shoulder pathologies in the process of diagnosing SIS.
Management
- Conservative management
- Physiotherapy.
- Platelet-rich plasma (PRP), stem cells, growth factors, and hyaluronic acid.
- Rest/Activity modifications.
- Operative management
- Subacromial decompression.
- Acromioplasty.
Anastasios M. Margaritis
Occupational Health& Safety Specialist.
Bsc Physiotherapy & Sports Science.
Orthopaedic Manual Therapist.
Back Mechanic Specialist.




